4 Ways to Maximize Your Chances of Prior Authorization Success
Navigating medication approvals can be tricky, but the VHAN Pharmacy Team offers practical tips to maximize likelihood of medication coverage. Here are four ways to improve the odds of prior authorization (PA) success:
1. Adhere to FDA-approved indications. Many payers limit coverage to approved indications. For older medications with many off-label uses, this can be challenging. Here are a couple of common scenarios:
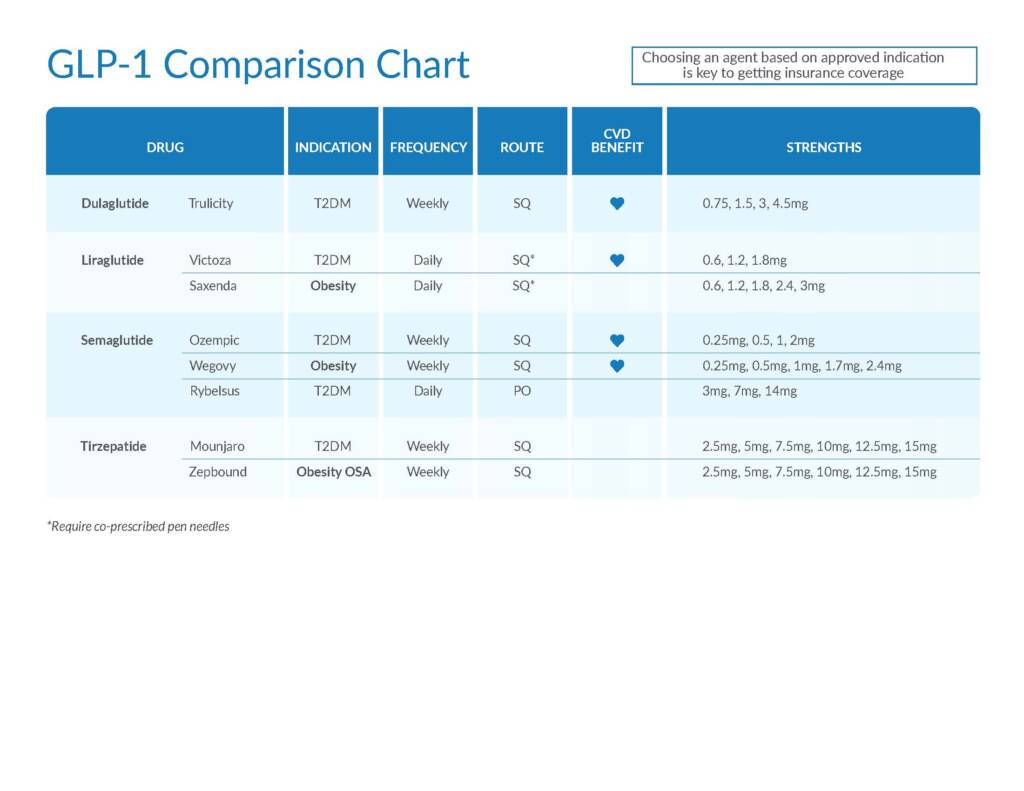
- Ozempic and continuous glucose monitoring will not be covered without diabetes. See chart below for comparison of GLP-1 agents.
- Lidocaine patches are often limited to neuropathic pain.
2. Document past trials, showing clear records of prior treatments. Plans often have preferred agents or require step therapy, such as “metformin before GLP-1s.” It’s valuable to have clear documentation of past therapies. It’s also helpful to explicitly note any contraindications, such as “cannot use phentermine due to hypertension.”
3. Highlight non-pharmacologic therapy. Prescriptions for semaglutide and tirzepatide products account for a large portion of PA requests. Many of these prescriptions are for weight loss. Almost universally, payers ask about past and ongoing behavioral modification, such as the magnitude of calorie restriction or hours of physical activity per week. Clear documentation of lifestyle changes and provider oversight help prevent additional questions, chart messages and appeals.
Non-pharmacologic therapy such as physical therapy can also be important for approval of overactive bladder treatments or muscle relaxers, for instance.
4. Ensure relevant diagnostics are completed. Payers have similar requirements, such as:
- Diabetes medications require A1c measurements.
- Weight loss medications require BMI numbers.
- Zepbound for obstructive sleep apnea requires a sleep study.
- Testosterone requires baseline levels.
Completing and documenting commonly required diagnostics, labs, etc. can prevent delays and improve quality of PA submissions.